Roohealthcare.com – Although optimal management of Chiari malformations remains elusive, suboccipital decompression has become a common surgical method for a variety of conditions. In the study, authors describe the results of the procedure in patients undergoing PCVR. Surgical techniques and imaging studies were analyzed to determine the success rate and the duration of follow-up. Here, we take a look at some of the pros and cons of this procedure.
Position of Surgical Procedure
The surgical procedure involves positioning the patient in a modified park-bench position. The surgeon and the assistant handling the instruments should stand across from each other and the anesthesiologist should be placed at the foot of the table. The surgeon makes an incision along the midline avascular fascial planes, aiming to access the suboccipital bone. The superior nuchal line muscles are separated from the underlying occipital bone with monopolar electrocautery.

The suboccipital region is located just lateral to the spinous process of C2. If a patient has pain in this region, a clinician should evaluate the suboccipital region as the cause of the pain. In patients with occipital neuralgia, the procedure may improve symptoms and reduce opioid consumption. It is important to note that suboccipital decompression is only effective for a limited number of patients.
Trapping the Nerves and Causing Various Clinical Manifestations
The risk associated with this procedure is low. Although surgery is an invasive procedure, it is not as high-risk as other surgical procedures. If you are undergoing this procedure, it is important to ask your physician about the risks and side effects of the surgery. Before the surgery, it is important to learn as much as possible about the skull and brain. They are in intimate relationship and contain numerous grooves and channels that accommodate the soft tissue of the brain.
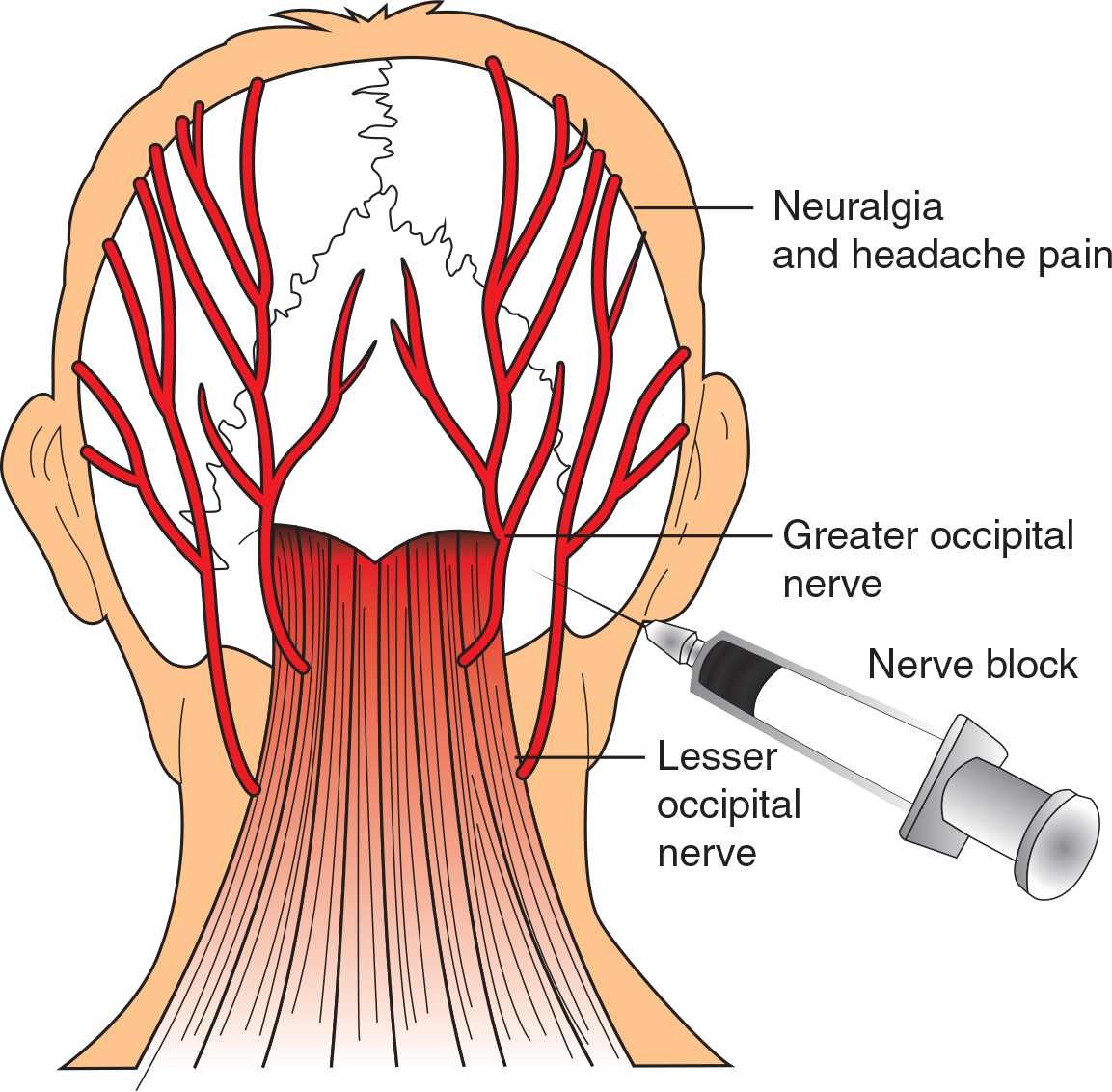
The greater occipital nerve is highly susceptible to trauma, and repetitive neck contractions can entrap it at the IOC muscle level. Once inflamed, the nerve may develop adhesions in the suboccipital area. Additionally, plastic surgeons “tuck” the skin around the lesser occipital nerve during cosmetic procedures. These procedures may entrap the nerves and lead to a variety of clinical manifestations.
Purpose of Chiari Decompression Surgery
The goal of Chiari decompression surgery is to stop the progression of the disease and alleviate symptoms. This surgery involves the removal of a small section of the skull to open the covering over the brain. A patch is then sewn on the skull, restoring the normal flow of spinal fluid. The patient will undergo periodic imaging tests to monitor the outcome of the surgery. The success rate of this procedure is very high.

Although the surgery can result in long-lasting neurologic effects, it has a relatively short recovery time. Patients typically feel temporary relief and are able to return to their daily activities. Although the procedure is relatively safe, the risks associated with this procedure are considerable. Sharp needles and intraneural injections are associated with increased risks of injury. A series of patients injected with particulate steroids had a “locked-in syndrome” that is attributed to the intraneural injections. Another study found that occipital nerve injections caused the delayed-onset respiratory arrest.
Reference: