Roohealthcare.com – The Tibial Collateral Ligament (TCL) is one of the four major ligaments in the knee. It spans the distance from the femur to the tibia and is attached to both ends of the tibia bone. Tibial collateral ligament injuries can be painful, and recovery can take months. Common sports that cause TCL pain include skiing and football. This ligament also stretches over the femur, attaching to the tibia bone and medial condyle.
Tibial Collateral Ligament Injury
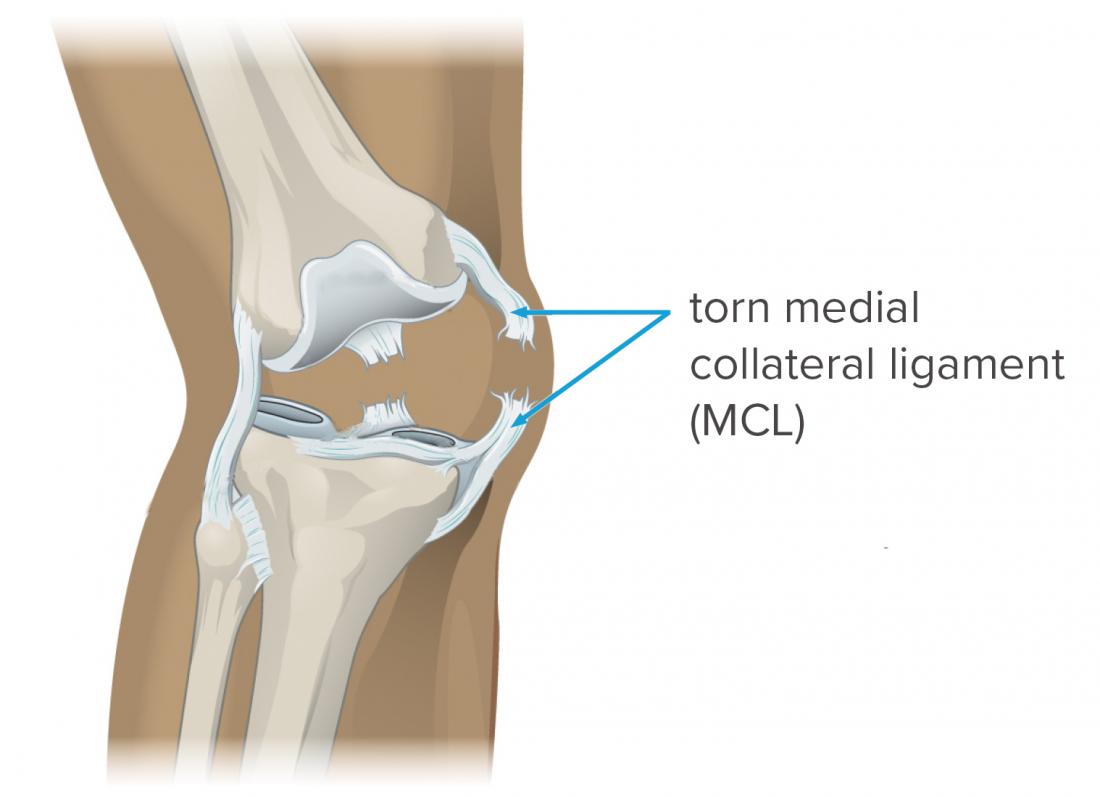
Injuries to the MCL are the most common type of TCL pain. Most often, the tear is at the top of the MCL, where it connects the tibia to the femur. The MCL is also known as the cruciate ligament, and it can be painful if it is stretched beyond its normal limits. TCL is often the source of a variety of other conditions, including arthritis, and TCL can also cause a range of symptoms.
TCL pain often affects people with sports activities. A tibial collateral ligament injury occurs when an athlete jumps or slides onto a hard surface. The injury will usually result in a popping sound and immediate pain around the inside of the knee. The MCL is made of fibrous tissue, and it connects the tibia and femur, making it vital for stability and mobility.
TCL injuries are not uncommon. In most cases, the tears are minor and require no surgery. Grade III tears often affect the tibia and femur. A thorough exam is necessary for determining whether a tibial collateral ligament injury requires surgery. If the MCL has ruptured throughout the entire superficial layer, however, surgery is recommended. A complete tear occurs when the MCL is torn.
Can Cause Knee Pain
The MCL is one of the four major ligaments in the knee. It connects the tibia to the femur, and is often injured while playing sports. It can cause knee pain, and can cause a popping sound. The MCL is made of strong, fibrous material that keeps the knee joint stable. It can cause an added degree of laxity. When the MCL is torn, the MCL can be painful.
A grade 1 MCL tear is not considered serious. This tear causes mild pain and tenderness. It takes about two weeks to heal. Several different treatment options are available. In some cases, a doctor will simply recommend surgery. Tibial Collateral Ligament tears may occur in any position. The MCL is a tough, flexible band of tissue located on the medial side of the knee. A rupture in the MCL can result in additional laxity.

A sprain or tear in the MCL is not a grade I or grade II injury. The condition is usually mild and is most often caused by a grade II or III tear. A patient suffering from a ruptured MCL should undergo a thorough examination to get a diagnosis and treatment. A physician can make a recommendation based on the symptoms and location of the pain. In many cases, the MCL is a small, thin band of fibers that connects the femur and the tibia.
TCL Tear May Have Tibial Collateral Ligament Fracture
A grade III MCL tear is often due to a severe injury to the MCL. Fortunately, most MCL tears are isolated and do not require surgery. Nevertheless, a grade III MCL tear can be unstable and cause laxity. It is important to note that a patient suffering from a TCL tear may have a fractured Tibial Collateral Ligament. Surgical repair is required for grade III if there is an incomplete ligament.
TCL is a tough band of fibrous tissue that stabilizes the knee. A grade I MCL tear causes an additional degree of laxity to the knee, which can lead to instability. Most MCL tears occur at the top of the MCL, while a grade II tear can cause more serious symptoms. A doctor may prescribe surgery to repair the MCL. The ligament can be replaced if it is damaged by a surgeon.

TCL pain may be a result of a sprain or a grade II MCL tear. Luckily, these MCL injuries are rare, and can be treated with proper rest. A simple MCL tear requires no surgery and is a mild tear that can be repaired by a surgeon. If the MCL is stretched or torn, it may require surgery to repair the joint. It will have to be reattached.
Reference: