Roohealthcare.com – Primary and secondary skin lesions are two types of abnormal growths of the skin. A primary skin lesion is present at birth, whereas a secondary lesion develops over time. The difference between the two is that a secondary lesion is the result of the underlying disease. Both lesions can be caused by various conditions. The most common lesions on the face include acne and moles. The latter is caused by deep, painful cysts or nodules.
Secondary Lesions can be Complications of the Disease Process
A secondary lesion can be either a lesion or a complication of a disease process. The former type usually occurs after a primary skin lesion has disappeared. Post-inflammatory hyperpigmentation is a secondary skin lesion and is also caused by a bacterial infection. The second type is more likely to be contagious and is more difficult to treat. While a secondary lesion is often a sign of an infection, a primary one is a precursor to cancer.
Secondary skin lesions are different from primary lesions. A primary skin lesion results in an underlying condition, such as an infection. A secondary skin lesion is the result of the progression or evolution of the primary. These lesions can be infected, or they can be post-inflammatory. They may appear as lattice-shaped or in patches. A secondary lesion can be painful and inflamed, or they can appear in a variety of forms.

Depending on the severity of the skin condition, secondary skin lesions are different from primary lesions. A secondary lesion is a complication of a primary one. A secondary lesion is a consequence of a secondary skin lesion. Typically, a primary lesion is the result of an inflammation. A primary skin disorder is the cause of a secondary one. A secondary lesion is a symptom of a complication.
The Best Way to Correctly Diagnose Secondary Lesions
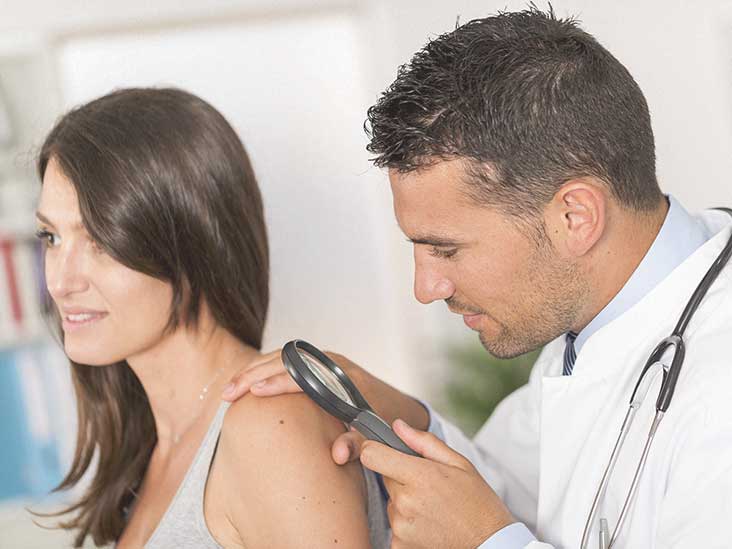
Secondary skin lesions are different from primary ones. The main difference is the type of skin lesions. A primary lesion is a normal, healthy skin condition. A secondary lesion is a complication of a primary lesion. A skin lession will be different from the surrounding one. This is why it is important to get a second opinion from a dermatologist. The best way to diagnose a secondary lesion is to see a doctor to have it looked at.
A secondary lesion can be any type of skin condition. There are many types of secondary skin lesions. Some of the most common are ulcers, keloids, and scars. However, it is important to note that the symptoms of a secondary lesion can range from being mild to being very serious. In most cases, the primary lesion will be the most prominent symptom, but a secondary lesion will be more likely to be more severe.

A secondary lesion is a skin condition that results in a secondary skin lesion. The difference between primary and secondary skin lesions is the type of change. A primary lesion is caused by a disease or injury, while a secondary one is a result of another condition. It is important to know what the differences are so that you can properly diagnose and treat it. There are also some differences between the two types of lesions, which can make them difficult to diagnose.
Secondary Lesions can be a Sign of an Disease or Infection
Primary and secondary skin lesions are different from the surrounding skin. A primary lesion is the result of a disease or injury, whereas a secondary lesion is the result of a reaction to a secondary lesion. Sometimes a secondary lesion can be a sign of a disease, or it may be a sign of an infection. Despite its names, these two types of lesions are different. While they are similar in appearance, primary lesions are usually more complex.
Primary skin lesions involve changes in the skin. A primary lesion is caused by a disease, whereas a secondary lesion is the result of a condition. A secondary lesion can be a symptom of an underlying disease, but it is not the same as a secondary one. The symptoms of a secondary skin lesion are not the same as those of a primary one. Hence, it is important to diagnose a lesion in order to treat it effectively.
Reference:
